What is a system? According to the Merriam-Webster dictionary, a system is defined as “a regularly interacting or interdependent group of items forming a unified whole.” You do not have to be an expert in system theory to understand that healthcare is a highly complex system, having many interrelated parts that make up the patient care process (diagnosis, testing, and treatment that are all done with many different caregivers in a variety of locations as well as multiple communication pathways between nurses, primary doctors, consulting doctors, technicians, etc.). While we know this is true, there is often a tendency, due to that very complexity, to do our improvement work in a silo. This brings significant risk of sub-optimizing the entire system by not appreciating the interdependencies inherent in patient flow to identify the true bottlenecks. This requires taking a comprehensive approach and identifying the connections and dependencies.
In this blog post, we will address some common mistakes in tackling patient flow and length of stay using a piecemeal, siloed approach.
Pitfall: Approach patient flow and LOS (length of stay) in a decentralized way with each unit/service working in its own silo
In many cases, hospitals see the problem through the lens of inpatient discharge time too late in the day, or that emergency department (ED) left without being seen rates are up because the ED is overcrowded with low-acuity patients. While these issues certainly impede patient throughput, often they are not the root causes but rather symptoms of bottlenecks further downstream. Working to change the discharge time or improve ED processes may help to some degree but will not have the full impact of identifying the bottlenecks and systemically and scientifically addressing the underlying causes.
Examples of flow stoppers that more accurately address the root cause issues are:
- Provider rounding schedules that restrict times patients are seen, assessed, and when orders are written
- Surgery schedules impacting demand on inpatient beds that are in competition with
ED admissions. - Ancillary and support department staffing on the weekends affecting testing, procedures, therapy, and administrative functions that impact timing of discharge and result in longer lengths of stay.
Because these are hard to tackle, we often work on efforts that are less political, implement plug-and-play solutions that feel like low-hanging fruit, or put pressure on nursing and ED teams to fix their processes because they are easier targets. We have all been here, and sometimes that is truly the only path forward...but as healthcare and process improvement professionals we must understand and acknowledge the limitations of this approach. We are missing the opportunity to truly transform our care processes to address the true barriers to flow.
Do instead: Take a system view, working across the continuum of care (including prehospital, home health, and primary care), mapping the entire value stream, with actual data, to find your real bottleneck(s).
Value stream analysis is an extremely effective way to scientifically improve systems and processes. A cross-functional team—comprised of staff from numerous departments and all levels of the organization, including nurses, physicians, ancillary staff, and leadership—will first seek to understand and document the current state through activities such as stakeholder interviews, Gemba walks, time observations, and process mapping. In addition, the team will collect actual data from the process, including how long each step takes to complete, how often each step is done right the first time, the length of delays that patients and staff experience, and more. From these activities, the team develops a current state map that highlights the waste, variation, and overburden in the system. Consequently, it makes visible to everyone where bottlenecks and opportunities for improvement truly exist.
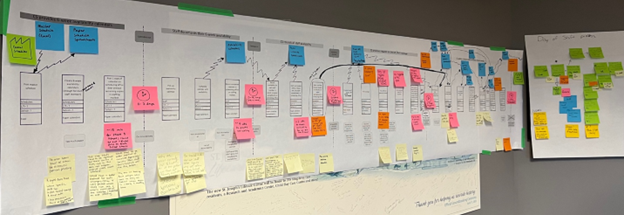
Next, the team will envision a future state—inspired by the ideal (safe, high quality, timely, waste-free)—which applies the Rules in Use to simplify pathways, fix connections, specify activities, and eliminate waste, variation, and overburden. For more information regarding this concept, refer to our last blog that introduced the Rules in Use). Future state mapping provides an improvement plan that targets the bottlenecks and key leverage points, which the organization aims to turn into reality within a specified time (often 3 months to 1 year).
This approach is superior to copy-and-pasting specific tools or best practices for multiple reasons. First, it allows you to target improvement to where it is truly needed in your organization. Secondly, because value stream analysis is done in a cross-functional way, it helps to align resources across the organization, preventing people from working in silos or not having what they need to drive improvement. Additionally, it involves data analysis and target setting, helping the organization to better measure and understand the impact of its improvement efforts.
Pitfall: Only improving direct patient care processes.
Another common pitfall many organizations succumb to is limiting their patient flow improvement efforts to the processes that physicians, nurses, and care managers engage with, such as admissions, care coordination, and discharge planning. While these processes certainly have the most impact on patient flow, there are several reasons not to overlook other processes.
First, this is part of thinking systemically, as described previously, and creating a culture of continuous improvement and habitual excellence. Paul O’Neill Sr. described habitual excellence as striving to be the best in the world at everything you endeavor to do. Along those same lines, to paraphrase Shigeo Shingo, your organization has not achieved a culture of continuous improvement until everyone, everywhere, every day is improving. Additionally, and more crucially at a tactical level, failing to address other processes means direct caregivers will continue to face frustrating and potentially unsafe distractions from providing excellent patient care.
How many times have you seen a nurse pulled away from a critical task because of a call bell to address an issue with a patient’s meal, or a physician having to walk halfway around the unit to find a computer with functional dictation? If you have spent any time observing processes on a patient care unit, you could cite dozens of examples of distractions and waste such as these. While these may not seem that significant on the surface, every time a caregiver is pulled away from their critical task, it raises the risk of harm or care being missed or delayed and can increase length of stay.
Do instead: Study and improve support services processes that ensure safe, effective care across all aspects of the patient’s stay.
Prisma Health CEO Mike Bundy compares nurses, physicians, and their support teams to special forces operators; what makes them excellent is when they can do the routine things well, without fail. Imagine what it could do for your hospital if nurses never had to answer call bells about things like, the pancake syrup the patient ordered is missing from their meal tray, or if the consultant physician could be confident the dictation system on every computer on the unit worked correctly. Improving these support processes—keeping the unit stocked with the right supplies in the right places, ordering and making patient meals, keeping software up to date and functional on unit computers, cleaning patient rooms in a timely manner, etc.—makes it easier for care teams to provide excellent patient care and reduces the risk of safety issues and care delays. Consequently, it is important to also investigate opportunities to improve support processes when working on patient flow.
Learn more about the “Pancake Syrup” approach.
Transforming how we care for patients by bringing new, creative solutions to the forefront requires the whole team to be engaged. The best way to ensure that happens is by taking a system view that includes a focus on both direct and indirect patient care processes. Using Value Capture’s principles-based, system-view approach, one client health system in the northwest US achieved 16-60% reduction in length of stay across numerous hospitals—without increasing readmissions—while saving more than $10 million! We invite you to share your wins and unique ideas resulting from taking a systemic approach with our improvement community.
This blog was a collaboration between Senior Advisors, Alison Hartman and Anthony Pepe.

Written by Value Capture, LLC
We are consultants who act as trusted advisors that guide health systems determined to produce perfect health with zero harm, wait, or waste — for patients, teams, and communities. We work with organizations by solving their biggest problem and doing it in a sustainable way, with “no tradeoffs” leading to exceptional change in organizations and the knowledge to continue to improve.

Submit a comment