Michael Bundy will be a presenter at "Leading with Safety: Accelerating towards Habitual Excellence," the intensive seminar that Value Capture and The Leapfrog Group are sponsoring at Duke University Health System, September 15-16, 2022. This seminar is designed specifically for healthcare executive leaders and Board members. Other presenters include Dr. Richard Shannon, CMO and CQO at Duke Health, and Leah Binder, President and CEO of The Leapfrog Group. Class size is limited to 15, so register today!
It was a treat to be able to help plan and host the first Value Capture webinar!
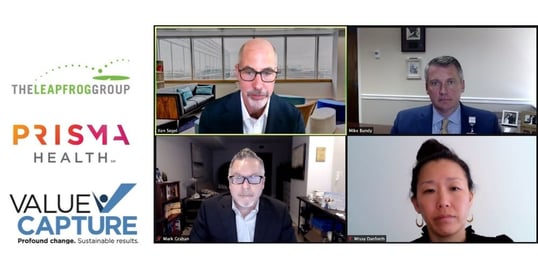
Ken Segel, our Value Capture CEO, and I were joined by Michael Bundy, Chief Executive Officer of Prisma Health Baptist Hospital and Prisma Health Baptist Parkridge Hospital, and Missy Danforth, Vice President of Health Care Ratings for The Leapfrog Group.
In this blog post, I wanted to share just a few highlights in case you missed the webinar.
Getting to the Root Cause of Being Hurried
Mike made a great point that the stated cause of many problems in healthcare was that people were hurried. This leads to quality problems, errors, and customer service complaints.
"The common theme that we've all heard in RCA after RCA is time. The common theme that we've all heard in RCA after RCA is time... let's address that time thing all the way down to the root cause. Let's remove as much of that consistent contributing factor to harm events as humanly possible."
Instead of stopping at "we were hurried," we have to keep asking "why?" Why were they hurried? We can address the causes of hurry. We can reduce the wasted motion and effort that causes hurry due to a lack of time to do the right things the right way.
"So we took that challenge from my new boss and from our learnings with Mr. O'Neill and at Baptist and Parkridge, we took it and we set out to define excellence with pancake syrup.
So let's think about the conundrum of time as it, as it links into harm events and all of the RCAs that many of us have had thought through and worked through over the years.
If a patient gets a breakfast tray and it has pancakes on it, but it doesn't have syrup, what does the patient do? Call bell, right?
And then a process failure in tray completeness has become a contributing factor to the caregiver's time issue. That's in every single RCA that we've all went through, the nurses now answering a call light calling dietary and delivering pancake syrup. If that nurse loses 10 minutes total because one tray was incomplete, then what other support and ancillary processes are impacting that time factor?
What if they never had to look two or three in two or three different Pyxis machines before each med pass? What if every supply was where it was supposed to be, was never stocked out in a machine?
What if they never waited on patient transport? What if the labs are always on the chart when the doctor's round and the nurse never has to call a physician for a decision that should have been made when the caregiver rounded, how much time could we give back to them?
And then how close to the theoretical limits could they execute nursing processes in with the time we gave them back? And what impact could that have on qualitative outcomes?
If we can simultaneously impact that time factor and have team members prove to themselves on the front line that zero process outliers is really possible in more rudimentary processes, the outcomes would be creating bandwidth for the hands-on patient care staff to do the same with more complex and patient facing processes."
I love how Mike states that. We can use proven improvement methodologies (he used the phrase "micro P.I." -- or process improvements) and Value Capture is well equipped to help organizations learn the habits and practices of improving the work systems -- and that starts with leadership and a compelling vision, as Mike articulates.
Raking Your Own Leaves First
An attendee asked a question:
"Do you have advice for how to engage physicians who are not employed by the hospital in this vitally important culture change?"
Mike's response included a colorful (fall colors?) analogy:
"So, we said when we started it, we were going to start as far away from the license as possible, right? We said that we're going to begin proving to ourselves that zero process failures is possible with food and nutrition services, environmental services, patient transport, and then we're going to work our way up into the ancillary and support services.
We likened it as to raking our leaves. You can't ask somebody else to rake the leaves in their yard until you've raked your own leaves. And so we're going to rake all the leaves as far away from the license as we can. And then we're going to work our way up to the, the ancillary work. And then we're going to work our way up to the licensed caregivers. And eventually when we have all of our leaves raked, you know, we're going to be able to go to our, to our medical staff.
And I'll get to the question about whether they're employed or not employed and just a second, but it's important.
You know, probably in my first week or two weeks, I went and I met with our hospitalist group on one of the two campuses who looked at me and said, "Please don't tell us to come write discharge orders earlier. Cause we'll write our discharge orders earlier and your staff will let the patient stay there all day."
And so we had to make sure we raked our leaves at the very granular level before we worked our way up through the licensing channels, to the physicians. And then, all of a sudden they were like the sea, and leaves getting raked around them and literally went, "We're going to have to get on board cause it's coming our way."
And in the question very specifically to whether or not the physician is part of the integrated delivery health network from an employed status, or whether they're in your network or whether they're just, or they're an exceptionally aligned private provider.
You know, I like to say, I just want to work with people that want to take incredibly good care of other people.
And when you connect this to purpose and the purpose is to patient, what I've found is that physicians, regardless of where their W2 comes from, wants to take great care of people.
And when you want to align behaviors behind the concepts that Mr. O'Neill used to say, it's one of my favorite Paul O'Neill-isms.
When you make it an inarguable argument, it doesn't matter where are whether or not they're employed or where they're out on the license change. It's now an inarguable argument because it's about somebody's safety, their quality outcome, their quality of life going forward.
And so, you know, it's not okay to not take exceptional care of people because that's what you signed up to do."
There's So Much More
This blog post just scratches the surface of what you'll get from this webinar. You'll hear more from Mike. You'll hear Missy Danforth give a good overview of the great work that Leapfrog Group does. Maybe we'll highlight more quotes in additional posts.
What do you think about these remarks? Feel free to post a comment, below.
If you like this post and want to get more content from Value Capture, subscribe to our new email notifications feature.
Related Post
Enjoyed this post? Read another post about the webinar:
Get the Full Recording

Written by Mark Graban
Mark Graban has served healthcare clients since 2005. Mark is internationally recognized as a leading author and speaker on Lean healthcare. His latest book is "The Mistakes That Make Us: Cultivating a Culture of Learning and Innovation."


Submit a comment